
Advanced Variable products with swatches
Products variations colors and images without any additional plugins.

Products variations colors and images without any additional plugins.
Metabolic health is the state of optimal functioning of your body’s biochemical processes that manage energy production, storage, and utilization. It encompasses how efficiently your body regulates blood sugar, lipids, and other biomarkers critical for preventing chronic diseases like diabetes, heart disease, and obesity. Achieving and maintaining metabolic health involves balanced nutrition, regular physical activity, and informed monitoring of key health markers. This section explores the definition of metabolic health, the role of genetic methylation tests, the impact of homocysteine levels, and the importance of a full blood panel for personalized health management.
Metabolic health reflects how well your body processes and uses energy from food. A metabolically healthy individual typically has optimal levels of blood glucose, triglycerides, HDL cholesterol, blood pressure, and waist circumference without relying on medications. According to research, only about 12% of American adults meet these criteria, highlighting the prevalence of metabolic dysfunction. Poor metabolic health increases risks for insulin resistance, type 2 diabetes, cardiovascular disease, and even cognitive decline.
Key aspects of metabolic health include:
Maintaining metabolic health requires a lifestyle that prioritizes whole foods, regular exercise, adequate sleep, and stress management. Monitoring biomarkers through blood tests is essential to identify imbalances early and tailor interventions.
Genetic methylation testing is crucial because it identifies variants in genes like MTHFR, COMT, and MTR that can impair methylation, potentially leading to health issues such as elevated homocysteine, mood disorders, or infertility. By understanding your genetic profile, you can personalize supplementation and lifestyle changes to optimize methylation and reduce disease risk.

Affects folate conversion to 5-MTHF (methylfolate). Key SNPs: C677T, A1298C.

Influences homocysteine-to-methionine conversion using 5-MTHF and B12. Key SNP: A2756G.

Supports MTR by regenerating methionine synthase. Key SNP: A66G.
Converts S-adenosylhomocysteine (SAH) to homocysteine. Less common but critical for preventing SAH buildup.

Regulates neurotransmitter (e.g., dopamine) breakdown via methylation. Key SNP: Val158Met. Some panels include additional genes like BHMT, CBS, or MAO, which also impact methylation or related pathways.

The MTHFR gene variant is a critical methylation factor because it impairs the body’s ability to process folate, potentially leading to elevated homocysteine levels and increased risks of cardiovascular and neurological issues. In America, where folic acid is widely added to processed foods like cereals and breads, this variant can exacerbate these risks due to the accumulation of unmetabolized folic acid.
Personalized nutrition optimizes health by tailoring diets to individual needs, emphasizing reduced sugar and carb intake to stabilize blood sugar and enhance metabolic efficiency. Cutting back on these can lower inflammation and support weight management, especially critical in America where processed foods dominate diets.
Impaired methylation is linked to cardiovascular disease, neurodegenerative disorders, and pregnancy complications due to its role in DNA methylation and homocysteine balance.
Supplementation aims to support methylation by providing cofactors (e.g., B vitamins) and methyl donors (e.g., SAMe) while addressing specific gene variants. Below are evidence-based strategies, but dosing and necessity depend on your genetic profile, homocysteine levels, and symptoms.




Homocysteine is a sulfur-containing amino acid produced during methionine metabolism, a process reliant on folate, vitamin B12, and B6. Normally, homocysteine levels are low (5–15 µmol/L), as it’s quickly converted back to methionine (remethylation) or cysteine (transsulfuration). Elevated homocysteine, or hyperhomocysteinemia (>15 µmol/L), is a biomarker of metabolic imbalance and a risk factor for multiple conditions.
Elevated homocysteine damages artery linings, promotes atherosclerosis, and increases blood clot formation, raising risks for heart attack (1.7 odds ratio), stroke (2.5 odds ratio), and peripheral vascular disease (6.8 odds ratio).
High levels are associated with cognitive decline, Alzheimer’s disease, and depression due to impaired methylation affecting neurotransmitter synthesis.
Homocysteine may reduce collagen stability, contributing to osteoporosis risk.
Elevated levels correlate with preeclampsia and neural tube defects, particularly in those with MTHFR variants.

Low B6, B12, or folate levels impair homocysteine metabolism, often correctable with supplements or dietary changes (e.g., leafy greens, eggs, fish).
MTHFR mutations or cystathionine β-synthase (CBS) deficiencies can elevate homocysteine, necessitating targeted supplementation like methylfolate.
Smoking, excessive alcohol, and sedentary behavior increase homocysteine, while exercise and a plant-based diet can lower it. A homocysteine test, typically a simple blood draw, helps assess risk. If levels are high, a healthcare provider may recommend B-vitamin supplements or dietary adjustments, though evidence on whether lowering homocysteine reduces cardiovascular events is mixed.
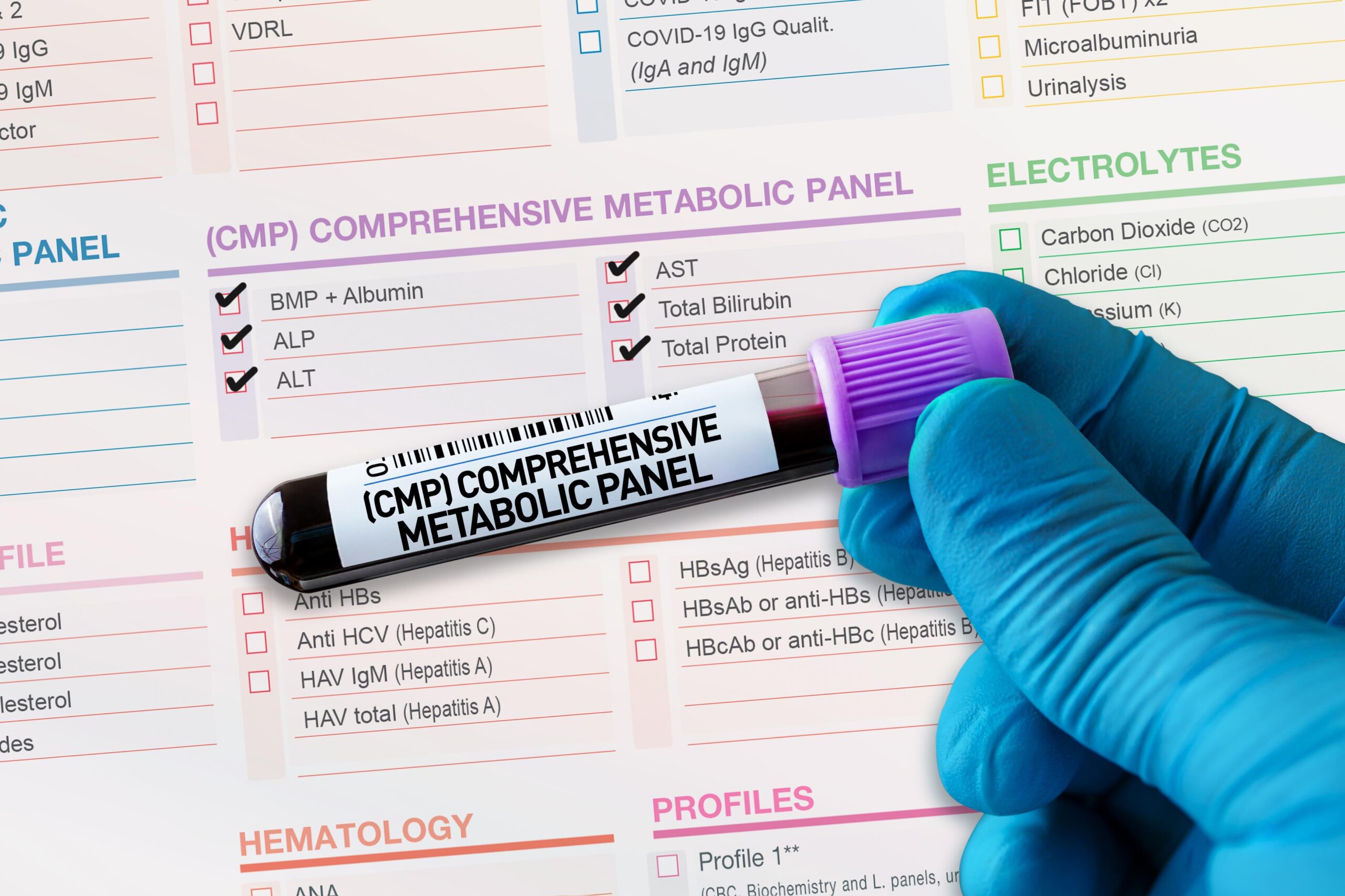
The first step to optimizing metabolic health is requesting a full blood panel from a healthcare professional. This comprehensive test provides a snapshot of your body’s biochemical status, identifying imbalances before symptoms arise. Regular monitoring empowers you to make data-driven decisions about diet, exercise, and supplements.

